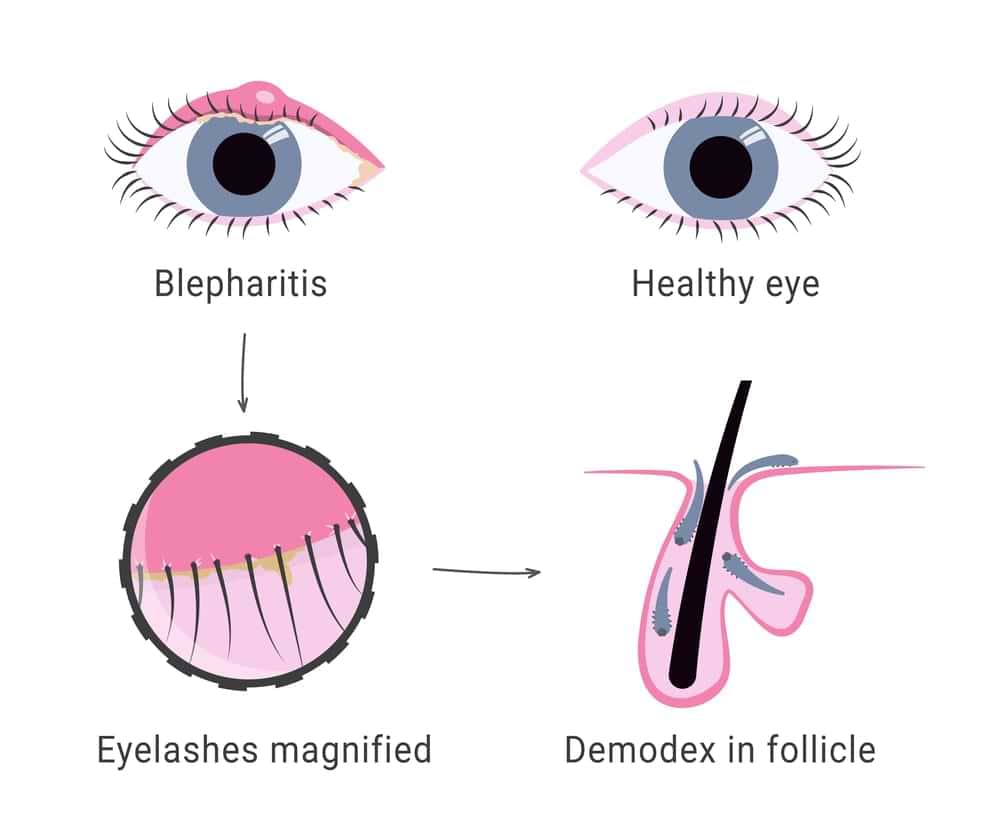
Do your eyelids often feel itchy, sore, or coated with crust in the morning? You may be dealing with blepharitis. This condition affects the eyelid margins and is one of the leading drivers of dry eye syndrome.
Many patients in Sydney live with burning, watering, or the constant feeling that something is in their eye. Left unmanaged, it can trigger styes, blurred vision, and ongoing discomfort. The good news is that with the right blepharitis treatment plan, symptoms can be controlled.
I’m David Truong, Owner and Principal Optometrist at Beyond Eyecare. Here are seven key facts on treatment that help.
Key Takeaways
- Blepharitis is chronic eyelid inflammation that often leads to dry eye, crusting, and persistent irritation.
- Common causes of blepharitis include rosacea, eczema, ageing, contact lens wear, Demodex mites, and environmental triggers like smoke or dust.
- Blepharitis diagnosis involves slit lamp examination, tear stability testing, eyelid swabs, and meibomian gland imaging.
- Treatment of blepharitis include eyelid hygiene, warm compresses, lid massage, medicated wipes, antibiotics, and in-practice therapies like BlephEx or thermal pulsation.
- Consistent eyelid care and regular optometrist reviews help reduce blepharitis flare-ups, manage symptoms, and maintain ocular surface health.
Understanding Blepharitis and Its Connection to Dry Eye
What is blepharitis? It’s a chronic inflammation of the eyelids that usually affects both eyes. Patients describe sensations of grit, soreness, or a foreign body in the eye. Redness, crusting, and morning stickiness are common. While rarely sight-threatening, it has a big impact on comfort and daily function.
How Blepharitis Relates To Dry Eye
One of the strongest connections between blepharitis and dry eye is meibomian gland dysfunction. These glands produce the oil that prevents tears from evaporating too quickly. Blockages and inflammation disrupt this balance, leading to unstable tears and chronic surface irritation. Patients with both conditions often experience more severe symptoms.
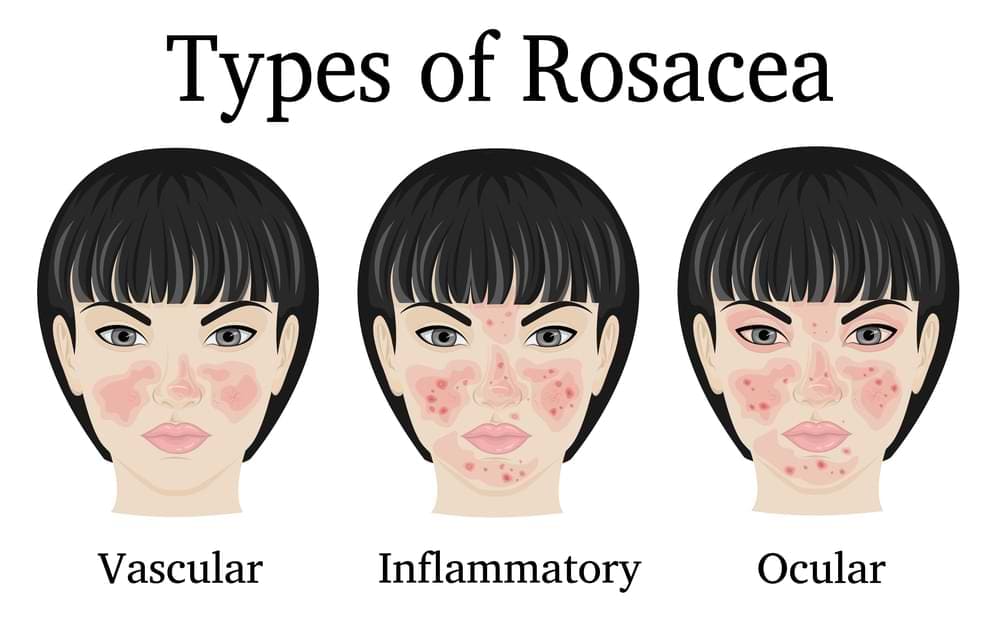
Types Of Blepharitis
Blepharitis can be classified into three types. Anterior blepharitis affects the base of the lashes, often tied to bacteria or seborrheic dermatitis. Posterior blepharitis involves the meibomian glands and is frequently linked to rosacea. Some people develop mixed or chronic forms that require combined treatment approaches.
Common Causes and Risk Factors
Ever wonder why your eyelids flare up at the worst possible times? From skin conditions like rosacea to long screen hours and even tiny mites, several hidden factors can trigger blepharitis.
Skin And Systemic Conditions
Skin and systemic conditions can set the stage for flare-ups. Rosacea, seborrheic dermatitis, and eczema are all known contributors. Autoimmune diseases such as Sjögren’s syndrome or rheumatoid arthritis raise the likelihood of chronic eyelid inflammation.
Lifestyle And Environmental Triggers
Lifestyle factors also play a role. Long hours of contact lens wear, hormonal shifts, and ageing increase the risk. Environmental triggers like smoke, dust, or long hours on digital screens add further stress. Diets low in omega-3 fatty acids are another overlooked contributor.
Infectious And Parasitic Factors
Infectious and parasitic factors are often underestimated. Overgrowth of bacteria at the lash line and infestations by Demodex mites living in lash follicles are common findings in chronic cases.
Recognising the Symptoms of Blepharitis
Do your eyes feel gritty, red, or swollen in the morning? These common signs of blepharitis often go unnoticed until daily comfort is affected.
Primary Symptoms
The most common symptoms are red, swollen, or itchy eyelids, crust around the lashes, and a gritty sensation. Symptoms are often worse in the morning.
Associated Eye Problems
Associated issues include blurred vision, sensitivity to light, and watery or frothy tears. Patients may also experience recurrent styes, chalazia, or chronic conjunctivitis. If blepharitis is left untreated, more serious complications can follow, including lashes turning inward and rubbing against the cornea.
Diagnosing Blepharitis and Dry Eye
Setting an appointment at our Sydney clinics may help reveal whether blepharitis, dry eye, or both are behind your symptoms.
Eye Examination Methods
We will conduct a thorough examination to separate blepharitis from other ocular surface diseases. A slit lamp allows close inspection of the eyelid margins, lashes, and tear film. Tear breakup time and osmolarity measurements provide insight into tear quality.
Additional Diagnostic Tools
We may use additional tools to make sure we get a proper diagnosis. These tools include eyelid swabs to rule out bacterial or mite infestations, and meibography to evaluate gland blockages or loss. Accurate diagnosis helps us guide effective treatment and prevents repeated cycles of discomfort.
Seven Key Facts About Blepharitis Treatment
Wondering what really works for long-term relief? From hygiene to advanced therapies, seven proven strategies can help calm eyelid inflammation and restore comfort.
| Fact | Treatment | How It Helps | Notes |
| 1 | Eyelid hygiene | Reduces bacteria, debris, mites | Daily routine, preservative-free wipes preferred |
| 2 | Warm compresses | Softens blocked oils | Use 2–5 minutes, warm flannel or heat mask |
| 3 | Lid massage | Restores tear film oils | Massage after heat for best effect |
| 4 | Medicated wipes/ointments | Removes bacteria and mites | Antibiotic ointments for anterior blepharitis |
| 5 | Antibiotics | Calms gland inflammation | Oral doxycycline or topical drops |
| 6 | In-office treatments | Clears deep blockages | BlephEx, IPL, thermal pulsation |
| 7 | Demodex therapies | Reduces mite infestations | Tea tree cleansers |
Fact 1: Eyelid Hygiene Is The Foundation Of Care
Daily cleaning of eyelid margins reduces bacteria, debris, and mite populations. Patients who follow a strict routine may have fewer flare-ups and more consistent relief. Options include cooled boiled water, preservative-free lubricating drops, or dedicated eyelid wipes. For sensitive skin, avoid harsh solutions like concentrated baby shampoo.
Fact 2: Warm Compresses Relieve Symptoms.
Applying gentle heat for two to five minutes may help soften the oils inside blocked glands. This makes expression easier and supports a healthier tear film. Simple methods include warm flannels or purpose-made heat masks.
Fact 3: Lid Massage Supports Oil Gland Function.
After heat, gentle massage could help express oils and restore the lipid layer. This is a key step in reducing evaporation, stabilising the tear film, and lowering irritation.
Fact 4: Medicated Wipes And Ointments Can Help
Commercial eyelid wipes remove bacteria and mites more effectively than soap. In cases of anterior blepharitis, prescription antibiotic ointments can reduce infection at the lash base.
Fact 5: Antibiotics May Be Needed In Some Cases
For stubborn or severe cases, oral antibiotics like doxycycline are used to calm inflammation caused by gland blockages. Topical antibiotics can target bacterial infection directly at the lid margins.
Fact 6: In-Office Treatments Clear Blocked Glands
Professional options provide longer-lasting relief than home therapy. BlephEx micro-exfoliation removes biofilm and bacterial debris. Thermal pulsation and intense pulsed light treatments target deep blockages and improve meibomian gland output.
Fact 7: Targeted Therapies Address Demodex Infestations
New treatments are emerging to directly target Demodex-related blepharitis, although availability varies between countries. In Australia, management often includes tea tree oil-based cleansers prescribed under professional guidance. Because tea tree oil can trigger allergic reactions, careful use and patch testing are recommended.
To learn more about some of the effective blepharitis remedies available, watch the following video by Dr Joseph Allen from the Doctor Eye Health YouTube Channel.
Advanced Blepharitis Care: Treatments and Daily Management
When blepharitis becomes stubborn or keeps coming back, the best results often come from combining professional treatments with consistent at-home care.
Treatment and management options include:
- In-office procedures such as BlephEx, thermal gland expression, or intense pulsed light to clear blocked glands and reduce recurring symptoms.
- Prescription therapies including steroid or cyclosporine eye drops for inflammation, or autologous serum drops in severe ocular surface disease.
- Daily lid hygiene morning and night, avoiding eye rubbing, and replacing eye makeup regularly.
- Managing flare-ups with warm compresses, extra lubricating drops, and pausing contact lens wear until symptoms ease.
- Preventing complications through regular check-ups to monitor tear stability, treat recurrent styes, and adjust care as needed.
With the right balance of professional treatment and daily routines, most patients find blepharitis manageable and are able to keep symptoms under control long term.
Frequently Asked Questions
What foods aggravate blepharitis?
Diets high in processed foods, sugar, and unhealthy fats can worsen inflammation, making blepharitis symptoms more noticeable. Some people also find dairy or alcohol aggravates flare-ups. In contrast, foods rich in omega-3 fatty acids, like salmon or flaxseed, may help support healthier eyelid oil glands and reduce irritation.
Is blepharitis always caused by mites?
No. While microscopic Demodex mites can contribute to blepharitis in some people, they are not the only cause. Blepharitis often develops from a combination of factors including blocked oil glands, bacteria, skin conditions, and allergies. Identifying the underlying cause helps guide the most effective treatment plan.
Is salt water good for blepharitis?
Using salt water at home is not recommended, as it can irritate the eyes and worsen dryness. Instead, warm compresses and medical-grade eyelid cleansers are safer and more effective. If needed, your eye doctor may also prescribe drops or ointments specifically designed to control inflammation and bacteria.
Is blepharitis caused by stress?
Stress does not directly cause blepharitis, but it can weaken the immune system and increase inflammation, making flare-ups more frequent or harder to control. People under high stress may also rub their eyes more often, worsening irritation. Good stress management, alongside proper eyelid hygiene, can reduce symptoms.
How do you cure blepharitis fast?
Unfortunately, there’s no instant cure for blepharitis. The condition is usually chronic and managed over time. Warm compresses, daily eyelid cleansing, and artificial tears can ease discomfort quickly, while prescription treatments may help in more stubborn cases. Consistent care is the key to long-term relief rather than a fast fix.
Final Thoughts
Blepharitis is a long-term condition, but it does not have to dominate your daily life. With the right combination of eyelid hygiene, home care, and professional treatments, symptoms can be controlled and comfort restored. The return on consistent treatment is clear vision, less irritation, and stronger quality of life.
If you are experiencing chronic eye irritation or dry eye syndrome in Sydney, come see us at Beyond Eyecare. Our team will assess your eyelids, your tear film, and your risk factors to create a blepharitis treatment plan that works for you.
Book an appointment with Beyond Eyecare today at Zetland (02) 9662 6364 or Surry Hills (02) 9556 1160. You can also schedule a convenient time through our website.
Therapeutical endorsement





